Britain's medicines regulator has authorized the world's first gene therapy treatment for sickle cell disease, in a move that could offer relief to thousands of people with the crippling disease in the U.K.
In a statement on Thursday, the Medicines and Healthcare Regulatory Agency said it approved Casgevy, the first medicine licensed using the gene editing tool CRISPR, which won its makers a Nobel Prize in 2020.
Casgevy — made by the Boston-based Vertex Pharmaceuticals (Europe) Ltd. and CRISPR Therapeutics — was approved by the agency for the treatment for patients with sickle cell disease and thalassemia who are 12 years old and over.
To date, bone marrow transplants, extremely arduous procedures that come with very unpleasant side effects, have been the only long-lasting treatment.
"The future of life-changing cures resides in CRISPR based (gene-editing) technology," said Dr. Helen O'Neill of University College London.
"The use of the word 'cure' in relation to sickle cell disease or thalassemia has, up until now, been incompatible," she said in a statement, calling the MHRA's approval of gene therapy "a positive moment in history."
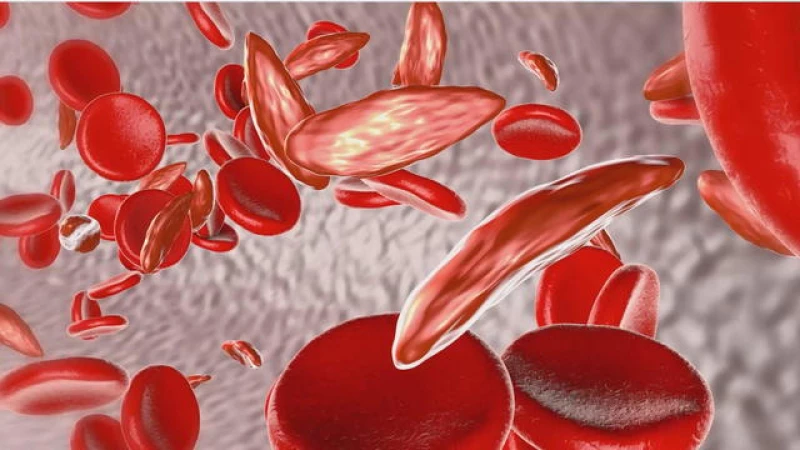
Both sickle cell disease and thalassemia are caused by mistakes in the genes that carry hemoglobin, the protein in red blood cells that carry oxygen.
In people with sickle cell — which is particularly common in people with African or Caribbean heritage — a genetic mutation causes the cells to become crescent-shaped, which can block blood flow and cause excruciating pain, organ damage, stroke and other problems.
In people with thalassemia, the genetic mutation can cause severe anemia. Patients typically require blood transfusions every few weeks, and injections and medicines for their entire life. Thalassemia predominantly affects people of South Asian, Southeast Asian and Middle Eastern heritage.
The new medicine, Casgevy, works by targeting the problematic gene in a patient's bone marrow stem cells so that the body can make properly functioning hemoglobin.
Patients first receive a course of chemotherapy, before doctors take stem cells from the patient's bone marrow and use genetic editing techniques in a laboratory to fix the gene. The cells are then infused back into the patient for a permanent treatment. Patients must be hospitalized at least twice — once for the collection of the stem cells and then to receive the altered cells.
Gene Therapy Treatments Could Become More Affordable
Gene therapy treatments have long been associated with exorbitant costs, making them inaccessible to those who would benefit the most. However, recent developments in Britain offer hope for a more affordable future.
Last year, a gene therapy for a fatal genetic disorder was approved in Britain with a staggering price tag of £2.8 million ($3.5 million). Recognizing the potential impact of this treatment, England's National Health Service (NHS) engaged in negotiations to secure a significant confidential discount, ensuring that eligible patients could access the therapy.
Vertex Pharmaceuticals, the company behind the gene therapy, has not yet determined the price for the treatment in Britain. However, they are actively collaborating with health authorities to expedite the reimbursement and accessibility process for eligible patients.
In Britain, medicines and treatments must receive approval from a government watchdog before they can be made available to patients in the national healthcare system. This ensures that all recommended treatments meet the necessary standards of safety and efficacy.
Casgevy is currently being reviewed by the U.S. Food and Drug Administration; the agency is expected to make a decision early next month, before considering another sickle cell gene therapy.
Millions of people around the world, including about 100,000 in the U.S., have sickle cell disease. It occurs more often among people from places where malaria is or was common, like Africa and India, and is also more common in certain ethnic groups, such as people of African, Middle Eastern and Indian descent. Scientists believe being a carrier of the sickle cell trait helps protect against severe malaria.